706
Views & Citations10
Likes & Shares
Introduction
and objective: We previously showed that inspiratory conductance
(IC) can be calculated from early inspiratory pressure fall and initial
acceleration of the inspiratory air column. To characterize IC further we
conducted a study to determine whether its value varies with height, weight,
BMI, age, sex and lung volumes.
Methods: We
measured IC, height, weight, FEV1, FVC and PEFR in 147 healthy volunteers’ age
18-50 years.
Results: During
tidal breathing at rest the mean (SD) IC was 8.31 (3.15) L s-1 kPa-1. No
significant correlation was found between IC and height (r=0.04), weight
(r=0.142), BMI (r=0.058), FEV1 (r=0.275), FVC (r=0.019), PEFR (r=0.182) or age
(r=0.017) and there was no significant difference between men and women. The
same was found for IC measured during slow deep breathing and rapid breathing.
Conclusion: IC is
independent of age, sex, height, weight, BMI and spirometric lung volumes so
there is no imperative to correct for those factors in an individual.
Within-subject directional changes in IC within the context of a short clinical
timeframe might be the best potential for clinical application.
Keywords:
Inspiratory conductance, Airflow resistance, Lung function, Spirometry
INTRODUCTION
In an earlier paper we published a
proof-of-concept study that described a novel apparatus to measure the
relationship between the initial drop in airway pressure and the acceleration
of the inspired air at the start of inspiration. The derived index, referred to
as inspiratory conductance (IC) has the units L.s-1 kPa-1
and can be posited as a potentially useful alternative to other measures of
airways status because it can be measured with little or no co-operation from
the subject [1]. It might therefore be of clinical value in patients who are
unconscious, for example in an intensive care setting or unable to perform
tests such as spirometry or whole-body plethysmography as is often the case in
people with cognitive impairment, particularly those with overt dementia.
The full conceptual, physiological and
technical background to IC is presented in depth in our previous papers [1,2].
In brief, IC is calculated from measurement of the maximum rate of pressure
fall (dP/dtmax) during very brief occlusion by a spring-loaded valve
at the onset of inspiration and the immediate maximum rate of acceleration of
the air column after the valve opens (dF/dtmax), then expressing
these as the ratio:
IC = dF/dtmax / dP/dtmax
=
L s-2/kPa s-1
=
L s-1 kPa-1 (the units of gas conductance in the airways)
Where F = flow (L-1), P = pressure
(KPa), t = time (s)
We conducted a study that showed IC to be a
stable, reproducible and consistent index in normal adult individuals and that
it showed the expected directional changes in response to externally applied
resistance to airflow [1].
There was a clear imperative to explore the
characteristics of IC further, particularly to establish whether it varied with
age, sex and stature, as do lung volumes measured by spirometry,
plethysmography or helium dilution. This was the logical next step because of a
need to determine if work would be required to set normative ranges for
between-subject comparative purposes in a population, and partly because we
observed no apparent differences between IC values in men and women in the
earlier small-scale study, which suggested the index does not vary with sex or
stature.
METHODS
Apparatus
We used the same
breathing apparatus described in the previous study, and the same calibration
routines. The only component to be replaced was the 12 V DC supply to the pressure
transducers to enable an even more stable pressure baseline and consistent
frequency response time. The digitization and analysis of the analogue signals
from the pressure transducers was also performed using the same sampling rate
and software (BioPac Systems, Goleta, CA, USA).
Spirometry to
measure peak expiratory flow rate (PEFR), forced expiratory volume in 1 s
(FEV1) and forced vital capacity (FVC) was performed with a Vitalograph®
Alpha 6000 spirometer (Vitalograph Ltd, Buckingham, UK) using standard
procedures [3].
Participants
147 healthy
volunteers (age range 18-50, 39 (26%) men) were recruited, all of whom were
staff or students at
Bournemouth University. A majority were either never-smokers or ex-trivial
smokers (estimated total exposure <1 pack year) and 13 (9%) current light
smokers (<10 pack years) were included. None had a history of diagnosed
asthma or any other significant respiratory disease, though 53 (36%) reported
occasional transient wheezing without dyspnea. All had otherwise negative
answers to the standard European Respiratory Society screening questionnaire
for respiratory disease [4]. The study was approved by the ethics subcommittee
of Bournemouth University and all subjects provided written informed consent.
Procedures
After spirometry the volunteers had their IC
measured using the same protocol as in the proof-of-concept study [1]. IC was
recorded during tidal breathing at rest, deep breathing at a rate of 6 breaths
per minute and voluntary rapid shallow breathing at a rate of 30 breaths/min.
Continuous data were tested 2-tailed for
significant difference using the Kolmogorov-Smirnov method and for correlation
using the Pearson method.
RESULTS
For the entire
group of subjects (n=147), the mean (SD) height was 168.27 (9.04) cm, weight
66.51 (18.0) kg, body mass index (BMI) 22.90 (3.78) kg m-2, FVC 4.24
(1.04) L, FEV1 3.51 (0.83) L, PEFR 449 (109) L min-1. The mean (SD)
IC values during tidal breathing at rest, slow deep breathing and rapid
breathing were 8.31 (3.15), 9.55 (3.44) and 18.33 (5.34) L s-1 kPa-1,
respectively. As found previously, IC during tidal breathing at rest and during
slow deep breathing showed no significant difference, whereas IC values rose
when the subject adopted rapid breathing. The most likely reason for this is
the more pronounced drop in intrathoracic pressure in the inspiratory phase
during rapid breathing which results in diffuse expansion of the airways and
therefore a transient drop in airways resistance at the time dF/dtmax
is being measured.
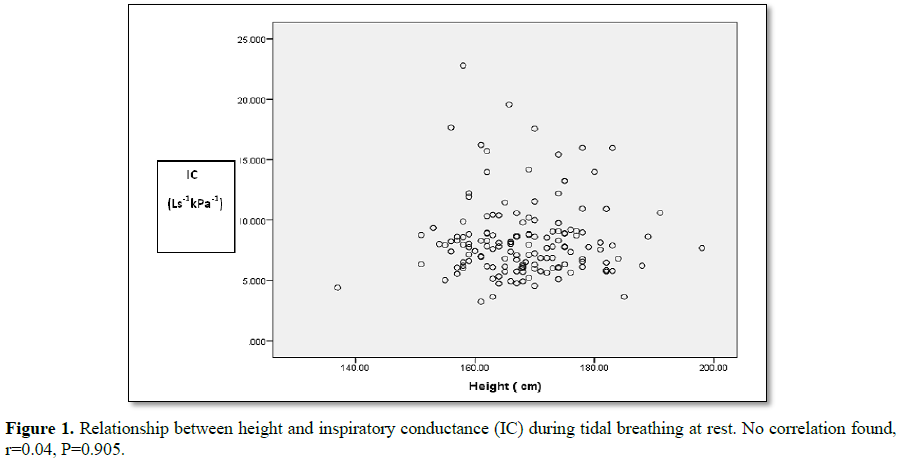
No correlation
(Pearson) was found between height and IC during any pattern of breathing. The
correlation coefficients (r) were: tidal breathing r=0.04, P=0.905 (Figure 1), slow deep breathing
r=-0.07, P=0.369, rapid breathing r=0.004, P=0.961. There was also no
significant correlation between IC and age (r=-0.017), weight (r=0.142), BMI
(r=-0.058), FVC (r=0.019), FEV1 (r=0.275) or PEFR (r=0.182) during tidal
breathing at rest and none in the other breathing patterns. There were no
significant differences in the mean IC values for men and women. Men and women
were found to have the expected differences in FVC and FEV1 which disappeared
when expressed as a percentage of the predicted value adjusted for sex, age and
height.
DISCUSSION AND CONCLUSION
This study
showed that IC was not related to sex, height, weight, BMI or lung volumes
measured by spirometry in healthy adults. There was also no apparent
relationship with age, though the age of the participants was not evenly
distributed across the age range, so further work might be needed to confirm
that finding. Therefore, unlike physiological indices that are clearly
influenced by body size and age, such as spirometric lung volumes, IC appears
not to need to be corrected for those factors. Potential clinical utility would
therefore lie in directional change of IC in an individual in a manner similar
to, for example, blood oxygen saturation. In the earlier study [1], we showed a
relatively low within-subject variation in IC in any given breathing pattern,
but considerable between-subject variation, as was the case in this study. This
finding also indicates greater clinical potential for within-subject comparison
use in short timeframe contexts. We now suggest that the behavior of IC as
measured by our method should be studied in a range of clinical settings to
position its usefulness as an indicator of changing respiratory physiological
status in patients with, for example asthma, acute bronchitis, chronic
obstructive pulmonary disease and pneumonia.
CONFLICTS
OF INTEREST
None
FUNDING
None
AUTHORSHIP
Stephen Allen:
Proposed original hypothesis, suggested the study, interpreted data, wrote
paper.
Debbie Gale:
Collected data, interpreted data, approved final draft.
Ahmed Khattab:
Suggested apparatus components, supervised data collection, approved final
draft.
Ian Brown: Built
apparatus and suggested improvements, interpreted data, approved final draft.
Jeff Bagust:
Analysed and interpreted data, supervised analytical software, approved final
draft.
1. Allen S, Brown I, Khattab A,
Bagust J (2011) Inspiratory conductance: An alternative index of the
relationship between inspiratory effort and airflow, with potential for
clinical use. Clin Resp J 6: 26-34.
2. Allen SC (2007) Inspiratory
transductance: A potential new measure of the relationship between inspiratory
force and the resistance to pulmonary airflow. Med Hypotheses 69: 287-292.
3. Miller MR, Hankinson J, Brusasco
V, Burgos R, Casaburi A, et al. (2005) Standardisation of spirometry. ATS/ERS
Task Force; standardisation of lung function testing. Eur Resp J 26: 319-338.
4. Burney PGJ, Luczynska C, Chinn S,
Jarvis D (1994) The European Community Respiratory Health Survey. Eur Resp J 7:
954-960.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- International Journal of Radiography Imaging & Radiation Therapy (ISSN:2642-0392)
- International Journal of Medical and Clinical Imaging (ISSN:2573-1084)
- International Journal of Diabetes (ISSN: 2644-3031)
- Journal of Oral Health and Dentistry (ISSN: 2638-499X)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Journal of Rheumatology Research (ISSN:2641-6999)